Credentialing with insurance companies allows telehealth practitioners to offer services to a broader patient base and provide smooth reimbursement for virtual consultations. Credentialing can be complex and time-consuming, especially for providers new to telehealth services. Here are a few tips to make the insurance credentialing process easier for telehealth providers:
Research Insurance Networks and Plans
Credentialing enables telehealth practitioners to accept insurance payments for virtual services, enhancing accessibility and affordability for patients seeking remote healthcare options. Before diving into the insurance credentialing process, telehealth providers must research various insurance networks and the plans they offer. Understanding the insurance landscape allows providers to focus on the networks that align with their telehealth services and patient demographics. By targeting the right insurance companies, telehealth practitioners can optimize their chances of successful credentialing and efficiently reach their target audience.
Gather Necessary Documents and Information
Credentialing requires telehealth providers to submit various documents and information to insurance companies. These may include licensure, certifications, educational transcripts, malpractice insurance, and proof of experience. Gathering all the necessary documents beforehand streamlines the credentialing process and prevents unnecessary delays. Because having all the required documents readily available streamlines the credentialing process and minimizes delays, it also enables telehealth providers to start offering virtual healthcare services sooner. Maintaining an updated and accurate set of credentials enhances the credibility and professionalism of telehealth practitioners. Up-to-date qualifications can foster trust among insurance companies and patients.
Telehealth providers must verify their professional information, including contact details and practice addresses, is consistent across all documents and servers. This consistency promotes clarity and avoids confusion during the credentialing process. Gathering and presenting the necessary information showcases the telehealth provider’s dedication to adhering to the healthcare industry’s regulations and guidelines. Comprehensive and well-organized documentation also demonstrates the telehealth provider’s commitment to meeting the stringent standards of insurance networks. This commitment can increase the likelihood of a successful credentialing process. Withholding necessary documents or submitting incomplete or outdated information can lead to unnecessary delays or even denial of credentialing.
Seek Guidance from Credentialing Experts
Navigating the insurance credentialing process can be overwhelming, especially for telehealth providers new to the virtual healthcare landscape. Seeking guidance from credentialing experts or professional services specializing in telehealth can be helpful. These experts understand the intricacies of telehealth credentialing, confirming that providers adhere to all necessary guidelines and requirements. Outsourcing your credentialing to a professional credentialing company helps simplify the process for telehealth providers.
Stay Organized and Proactive
Telehealth providers should maintain a comprehensive checklist of all required documents, deadlines, and follow-up dates. Staying on top of the process helps avoid missed opportunities and supports the credentialing journey to progress smoothly. Telehealth providers should also make sure their professional information, including contact details and practice address, is up-to-date and consistent across all documents and online platforms. Consistency in information avoids confusion during the credentialing process and helps establish credibility with insurance companies.
The insurance credentialing process for telehealth providers may present challenges such as prolonged approval times or unexpected denials. Anticipating and being prepared for such obstacles can reduce frustration and enable providers to address issues promptly. Persistence and clear communication with insurance companies is key to overcoming challenges and obtaining successful credentialing.
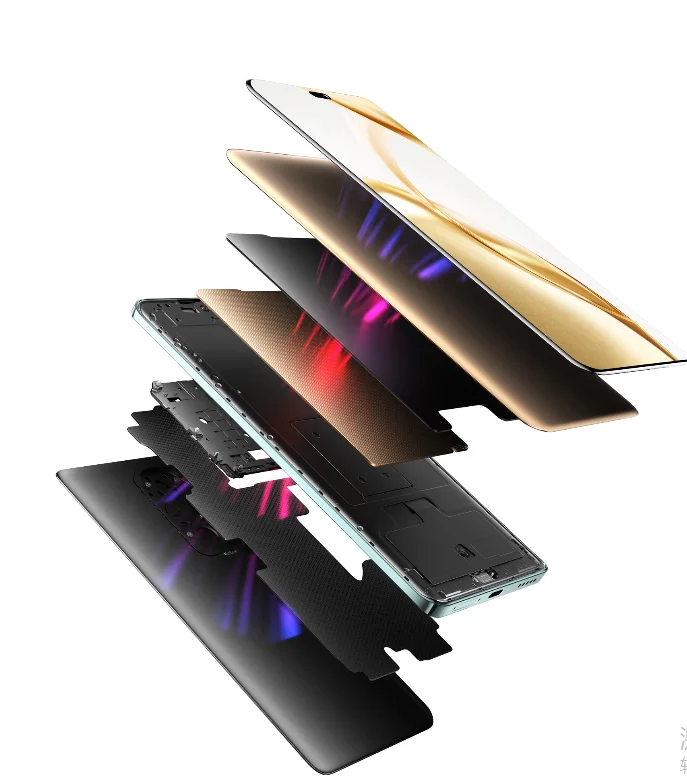
Utilize Technology for Credentialing
Incorporating technology can significantly streamline the insurance credentialing process for telehealth providers. Utilize telehealth software or electronic credentialing platforms to submit documents securely and efficiently. Technology simplifies the process, enabling providers to focus more on delivering quality telehealth services. Technology can assist in verifying that all submitted information is accurate and up-to-date, minimizing the risk of errors or discrepancies that could lead to credentialing delays or denials.
Electronic platforms often offer built-in validation tools that help telehealth providers meet all insurance company requirements before submission, increasing the chances of successful credentialing. The efficiency and convenience provided by technology enable telehealth providers to focus more on delivering high-quality virtual healthcare services and less on administrative tasks related to the credentialing process. Electronic credentialing can also reduce paperwork and manual data entry, freeing up valuable time for telehealth practitioners to attend to their patient’s needs.
Find an Insurance Credentialing Company You Can Trust
By dedicating time to online research, you can find an insurance credentialing company you can trust. Credentialing companies can help your credentialing process become more efficient, leading to successful participation in insurance networks. Speak with a quality credentialing company today to learn more about their services and how they can help you with credentialing.